Patient information on Obstructive Sleep Apnoea (OSA) – Part II
Who is this information for?
This information is for patients, families and carers of patients with Obstructive Sleep Apnoea.
How is OSA treated?
- Sleep apnoea is best treated by a knowledgeable sleep medicine specialist, in collaboration with your GP and often, an ENT surgeon.
- Goal of Treatment: maintain an open airway during sleep.
- Effective Treatment will:
- eliminate the symptoms of sleep disturbance.
- reduce the long-term health consequences.
- Most non surgical treatments require nightly use.
- The challenge for the clinician and the patient is to select an effective therapy that is appropriate for the patient’s problem and that is acceptable for long term use.
Read Obstructive Sleep Apnea (OSA) – Part I
- Lifestyle Changes
- Improve sleep hygiene
- Try to have a regular sleep time, and obtain an adequate amount of sleep every night (this varies from person to person)
- Minimise pre sleep activities such as TV, exercise
- Adjust sleep position
- Adjusting sleep position (to stay off the back) may help improve sleep quality in people who have OSA when sleeping on the back.
- However, this is difficult to maintain throughout the night and is rarely an adequate solution in isolation.
- Weight loss
- Weight loss may be helpful for obese or overweight patients.
- Weight loss may be accomplished with dietary changes, exercise, and/or surgical treatment.
- However, it can be difficult to maintain weight loss; the five-year success of nonsurgical weight loss is only 5 percent, i.e. 95 percent of people regain lost weight.
- Avoid alcohol and other sedatives
- Alcohol can worsen sleepiness, potentially increasing the risk of accidents or injury.
- People with OSA are often counseled to drink little to no alcohol, even during the daytime.
- Similarly, people who take anti-anxiety medications or sedatives to sleep should speak with their healthcare provider about the safety of these medications.
- Personal and public safety
- People with OSA must notify all healthcare providers, including surgeons, about their condition and the potential risks of being sedated.
- People with OSA who are given anesthesia and/or pain medications require special management and close monitoring to reduce the risk of a blocked airway.
- People with untreated OSA and daytime symptoms of fatigue should consider the safety of themselves and others if they operate heavy machinery or drive commercial vehicles as part of their employment. They may need to refrain from such activities and notify their employer until their OSA is adequately treated.
- Improve sleep hygiene
- Devices:
- Continuous positive airway pressure (CPAP)
- The most effective treatment for sleep apnea uses air pressure from a mechanical device to keep the upper airway open during sleep.

- A CPAP (continuous positive airway pressure) device uses an air-tight attachment to the nose, typically a mask, connected to a tube and a blower which generates the pressure. Devices that fit comfortably into the nasal opening, rather than over the nose, are also available.
- CPAP should be used any time the person sleeps (day or night).
- The CPAP device is usually used for the first time in the sleep lab, where a technician can adjust the pressure and select the best equipment to keep the airway open.
- Alternatively, an “auto” device with a self-adjusting pressure feature, provided with proper training, can get treatment started without another sleep test.
- While the treatment may seem uncomfortable, noisy, or bulky at first, most people accept the treatment after experiencing better sleep.
- However, difficulty with mask comfort and nasal congestion prevent up to 50 percent of people from using the treatment on a regular basis.
- Continued follow up with a healthcare provider helps to ensure that the treatment is effective and comfortable.
- Information from the CPAP machine is often used by physicians and therapists to track the success of treatment.
- CPAP can be delivered with different features to improve comfort and solve problems that may come up during treatment. Changes in treatment may be needed if symptoms do not improve or if the person’s condition changes, such as again or loss of weight.
- The most effective treatment for sleep apnea uses air pressure from a mechanical device to keep the upper airway open during sleep.
- Dental devices
- A dental device, called an oral appliance or mandibular advancement device (MAD), can reposition the jaw (mandible), bringing the tongue and soft palate forward as well. This may relieve obstruction in some people
 This treatment is excellent for reducing snoring, although the effect on OSA is sometimes more limited.
This treatment is excellent for reducing snoring, although the effect on OSA is sometimes more limited.- As a result, dental devices are best used for:
- mild cases of OSA when relief of snoring is the main goal.
- Failure to tolerate and accept CPAP is another indication for dental devices.
- While dental devices are not as effective as CPAP for OSA, some patients prefer a dental device to CPAP.
- Side effects of dental devices are generally minor but may include changes to the bite with prolonged use, and TMJ dysfunction.
- Continuous positive airway pressure (CPAP)
- Surgical treatment
- Sleep Apnoea Surgery is generally reserved for patients who cannot tolerate or do not improve with non-surgical treatments such as CPAP or oral devices. Read information about Discharge Information: Post Neck Surgery
- Surgery can play an important role in the management of obstructive sleep apnoea (OSA).
- Surgery may be indicated in select OSA patients who have:
- An inability to tolerate adequate CPAP or other device treatments
- Ongoing OSA despite adequate CPAP treatment
- Additional upper airway symptoms such as – recurrent tonsillitis, or nasal obstruction.
- The nature of the surgery considered/offered depends on:
- Severity of OSA
- Anatomical level of obstruction – e.g. palate, vs tongue, vs pharynx.
- Therefore, upper airway surgery in patients with OSA requires a complete anatomical examination, including trans-nasal flexible laryngoscopy, sometimes Drug-induced sleep endoscopy (DISE) and cranio-facial and upper airway imaging.
- Surgical procedures can reshape structures in the upper airways such as the nasal passages, soft/hard palate, tongue and tonsillar tissue. Procedures can also surgically reposition the facial bones.
- Surgeries can include:
- Nasal surgery: e.g. Septoplasty, Turbinate reduction
- As a single intervention, nasal surgery does not reliably treat OSA
- The primary goal of nasal surgeries in the context of OSA is to improve CPAP, oral appliance, or other surgery effectiveness in selected patients affected by nasal obstruction.
- Palate surgery: e.g. Uvulopalatopharyngoplasty (UPPP), tonsillectomy
- Most common surgical procedure for OSA
- UPPP frequently improves both the physiological abnormality of OSA and the clinical symptoms, but benefit is variable, and cure is rare.
- Lower Pharyngeal and laryngeal procedures:
- Tongue reduction: midline glossectomy, lingualplasty, lingual tonsillectomy, radio-frequency tongue volume reduction
- Tongue advancement/stabilisation: genioglossus advancement, hyoid suspension, tongue suspension, mandibular advancement
- Epiglottis correction: Epiglottopexy, Hyoid suspension
- Global upper airway procedures: include 3 diverse procedures, each with specific indications, that can improve the upper and lower pharyngeal airway globally or bypass the upper airway; they are not site directed and include:
- Maxillo-mandibular advancement: Projects the entire lower facial skeleton and attached tissues forward; it’s
- Tracheotomy: bypasses the upper airway entirely by placing a breathing tube through the front of the neck
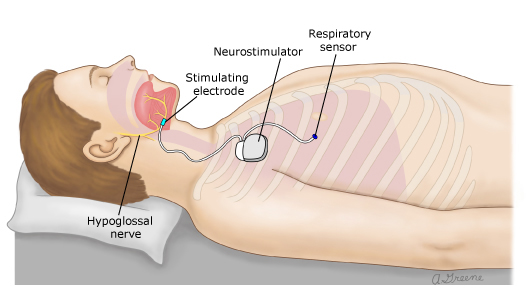
- Upper airway stimulation – e.g. Inspire® hypoglossal nerve stimulation
- The upper airway is stimulated via an implantable neurostimulator device which activates muscles in the tongue, timed with breathing muscles, to open the lower pharyngeal airway, preventing it from collapse. It’s availability
- Nasal surgery: e.g. Septoplasty, Turbinate reduction
- Surgical treatment for OSA can provide long-term benefits in selected patients.
- Although, complete elimination of OSA is often not achieved, and relapse of symptoms after a few years
Concerns or questions?
You can contact your ENT Specialist at the Melbourne ENT Group (MEG):
- Phone: 1300- 952-808
- Email: admin@melbentgroup.com.au
- Website: www.melbentgroup.com.au
Assessment by Respiratory/Sleep Medicine Physician is also recommended.
Your GP is also the best contact for ongoing care and concerns.