Chronic Rhinosinusitis and Sinus Infections
Who is this information for?
This information is for patients and carers of individuals who have Chronic Rhino-sinusitis
Chronic Rhino-Sinusitis Overview
- The sinuses are hollow air pockets in the bones of the face and head that probably exist to cushion the brain during trauma
- The sinuses are lined with a thin layer of tissue that normally makes a small amount of mucus to keep the sinuses healthy and lubricated and flush away germs.
- Rhinosinusitis occurs when the lining of the sinuses gets infected or irritated, become swollen, and create extra mucus.
- The swollen lining may also interfere with drainage of mucus.
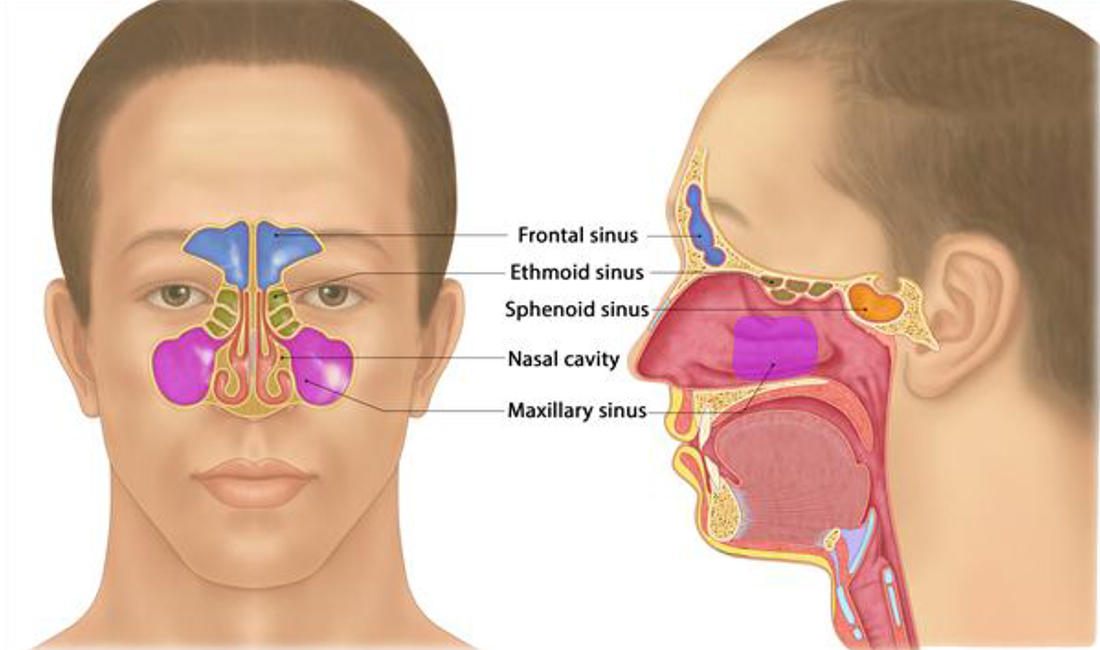
Sinuses of the Face
- Chronic rhinosinusitis refers to a condition that lasts at least 12 weeks despite being treated and causes at least TWO of the following symptoms:
- Nasal congestion
- Mucus discharge from the nose or mucus that drips down the back of the throat
- Facial pain, pressure, or “fullness”
- A decreased sense of smell. Read information about Anosmia or decreased sense of smell.
- Chronic rhinosinusitis is different from the more common form of rhinosinusitis (called acute rhinosinusitis), which is a temporary infection of the sinuses that often occurs following colds. Chronic rhinosinusitis is a more persistent problem that requires a specific treatment approach.
- It is sometimes overlooked by both patients and healthcare providers because the symptoms are more low grade and chronic
- If you have been treated for rhinosinusitis with antibiotics multiple times within a single year, or if you have two or more of the symptoms listed above much of the year, talk to your healthcare provider about whether you might have chronic rhinosinusitis.
Chronic Rhino-Sinusitis Causes
- Unlike acute rhinosinusitis, which is usually caused by infection, chronic rhinosinusitis often has more complicated and elusive causes.
- Infections can certainly contribute to or worsen chronic rhinosinusitis, but people with the chronic condition usually have longstanding inflammation that cannot be explained by infection alone
- Healthcare providers often divide chronic rhinosinusitis into three different categories, depending upon the features that are present.
- Chronic rhinosinusitis without nasal polyposis
- Chronic rhinosinusitis without nasal polyposis is the most common type of rhinosinusitis.
- In this form of rhinosinusitis, the swelling and irritation of the sinus lining may be caused by different factors, such as allergies to things in the air, irritation from things in the air, and infections (figure 2).
- The factors are different in different people.
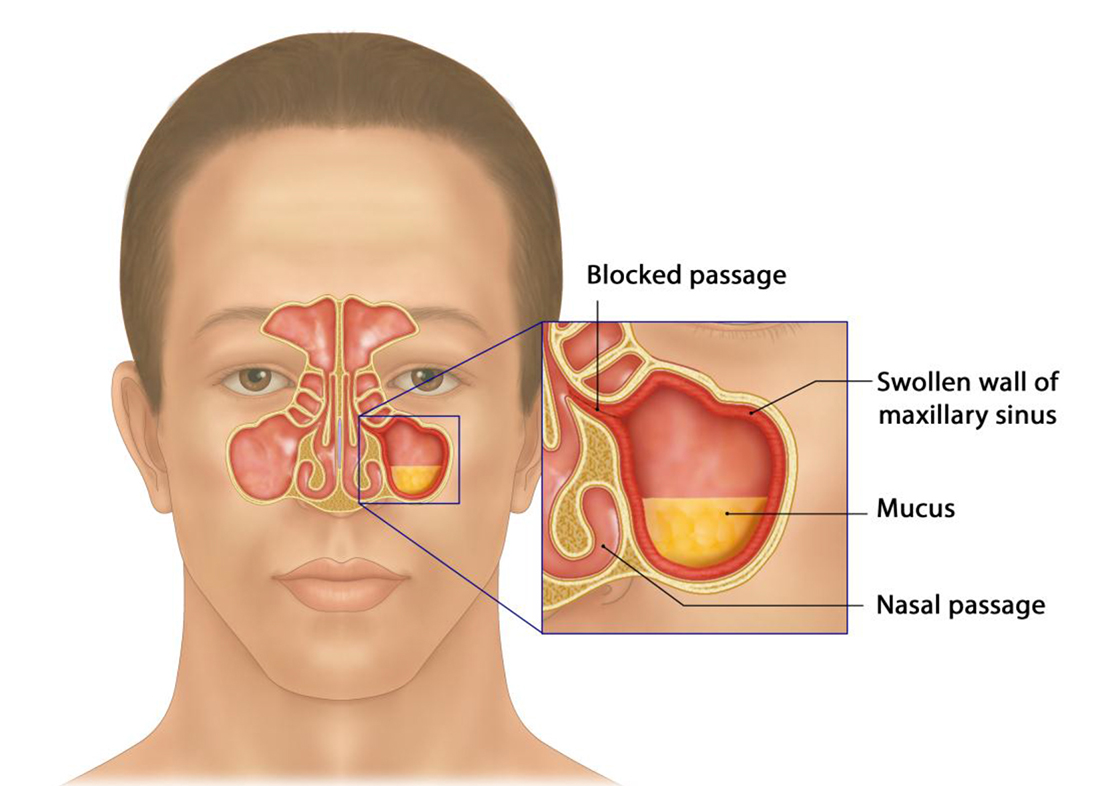
Development of Sinusitis – the sinuses becomes swollen due to inflammation, blocking
the passage, and leading to mucus build-up
- Chronic rhinosinusitis with nasal polyposis
- Some people with chronic rhinosinusitis have abnormal soft, jelly-like growths inside their nose or sinuses called nasal polyps.
- The polyps can become large and numerous enough to clog the sinuses, causing symptoms.
- Scientists do not fully understand why some people form nasal polyps. Treatment involves medications to shrink the polyps or surgery to remove them. Some people need both.
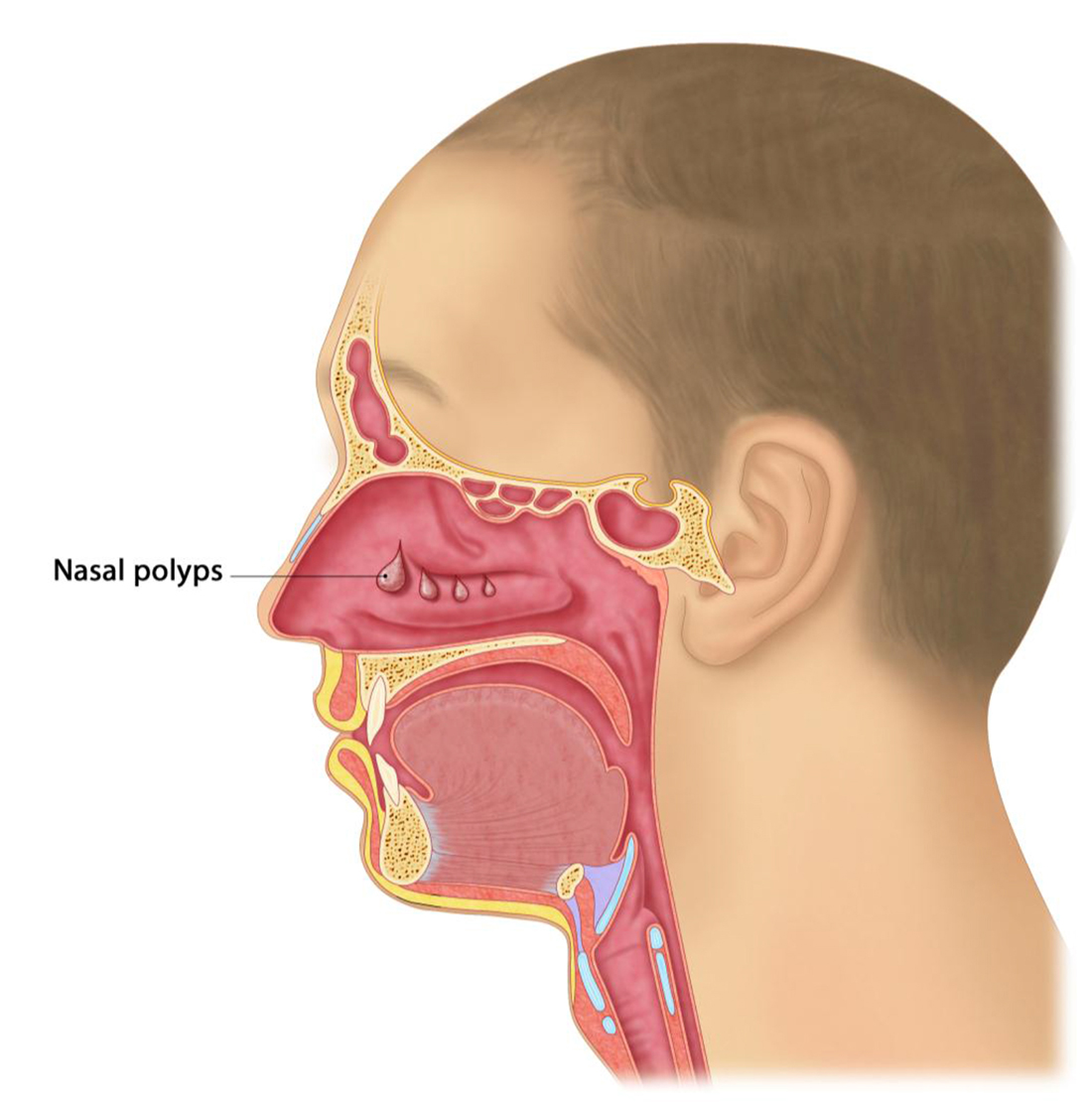
Example of Sinuses with nasal polyps
- Chronic rhinosinusitis with fungal allergy (“allergic fungal rhinosinusitis”)
- Some people with chronic rhinosinusitis develop a strong allergic response to fungi (the plural of fungus) inside their sinuses.
- It is normal for air to contain small amounts of fungi (airborne spores), and most people can breathe in air containing fungal spores without problems.
- However, in some people, the allergy to fungi causes the sinus lining to make thick, dense mucus that fills the sinuses.
- To diagnose this type of chronic rhinosinusitis, a healthcare provider must find thick mucus in the sinuses, see fungi in the mucus under the microscope, and show (with allergy testing) that patients are allergic to fungi. (See “Allergic fungal rhinosinusitis”.)
Chronic Rhino-sinusitis Risk Factors
- Several factors can increase your risk of chronic rhinosinusitis or worsen your symptoms once you have the disorder.
- These include:
- Allergies: Allergies are much more common among people with chronic rhinosinusitis than they are among people in the general population. This is especially true of allergies that are present year-round, such as dust mites, animal dander, moulds, and cockroaches. Allergies that are poorly controlled can worsen the symptoms of chronic rhinosinusitis. (See “Patient information: Allergic rhinitis (seasonal allergies) (Beyond the Basics)”.)
- Exposure to tobacco smoke or airborne irritants: Exposure to cigarette smoke or certain environmental toxins, such as formaldehyde, can increase the risk of chronic rhinosinusitis.
- Immune system disorders: Most people with chronic rhinosinusitis have normal immune systems. However, people with certain immune system problems are at increased risk of chronic rhinosinusitis. They may also have recurrent problems with other infections, such as ear and chest infections
- Viral infections: Some people develop chronic rhinosinusitis after having repeated viral infections (such as the common cold), although it is not clear that the infections actually cause the chronic rhinosinusitis.
- Deviated septum & enlarged turbinates:
- The piece of cartilage that runs down the midline of the nose and separates the nostrils, called the septum, is not entirely straight in many people. This is a condition called a deviated septum. This may be present from birth or develop later in life as the result of injury to the nose. A deviated septum may cause one nostril to be blocked, but it usually does not cause chronic rhinosinusitis.
Chronic Rhino-sinusitis Symptoms:
- As noted above, the symptoms of chronic rhinosinusitis must include two or more of the following:
- Nasal congestion
- Mucous discharge from the nose or mucus that drips into the back of the throat
- Facial pain, pressure, or “fullness”
- A decreased sense of smell (which is especially common among people who have polyps)
- Many people with chronic rhinosinusitis also experience fatigue, although this symptom is not used to diagnose chronic rhinosinusitis, because there are many other causes of fatigue unrelated to conditions of the sinuses. Still, fatigue is a prominent feature of chronic rhinosinusitis, and it can be the most difficult symptom for some people to manage.
Chronic Rhino-sinusitis Diagnosis:
- Chronic rhinosinusitis is likely if a person has had two or more of the symptoms listed above for a period of at least three months
- In addition, there should be evidence of sinus disease that can be seen on:
- Sinus Computed Tomography (CT) scan
- A sinus CT scan is a procedure that takes about 15 minutes and involves a series of radiographs of the head and face. The radiographs give a detailed picture of the linings of the sinuses and any mucus or polyps within the space of the sinuses.

- A sinus CT scan is a procedure that takes about 15 minutes and involves a series of radiographs of the head and face. The radiographs give a detailed picture of the linings of the sinuses and any mucus or polyps within the space of the sinuses.
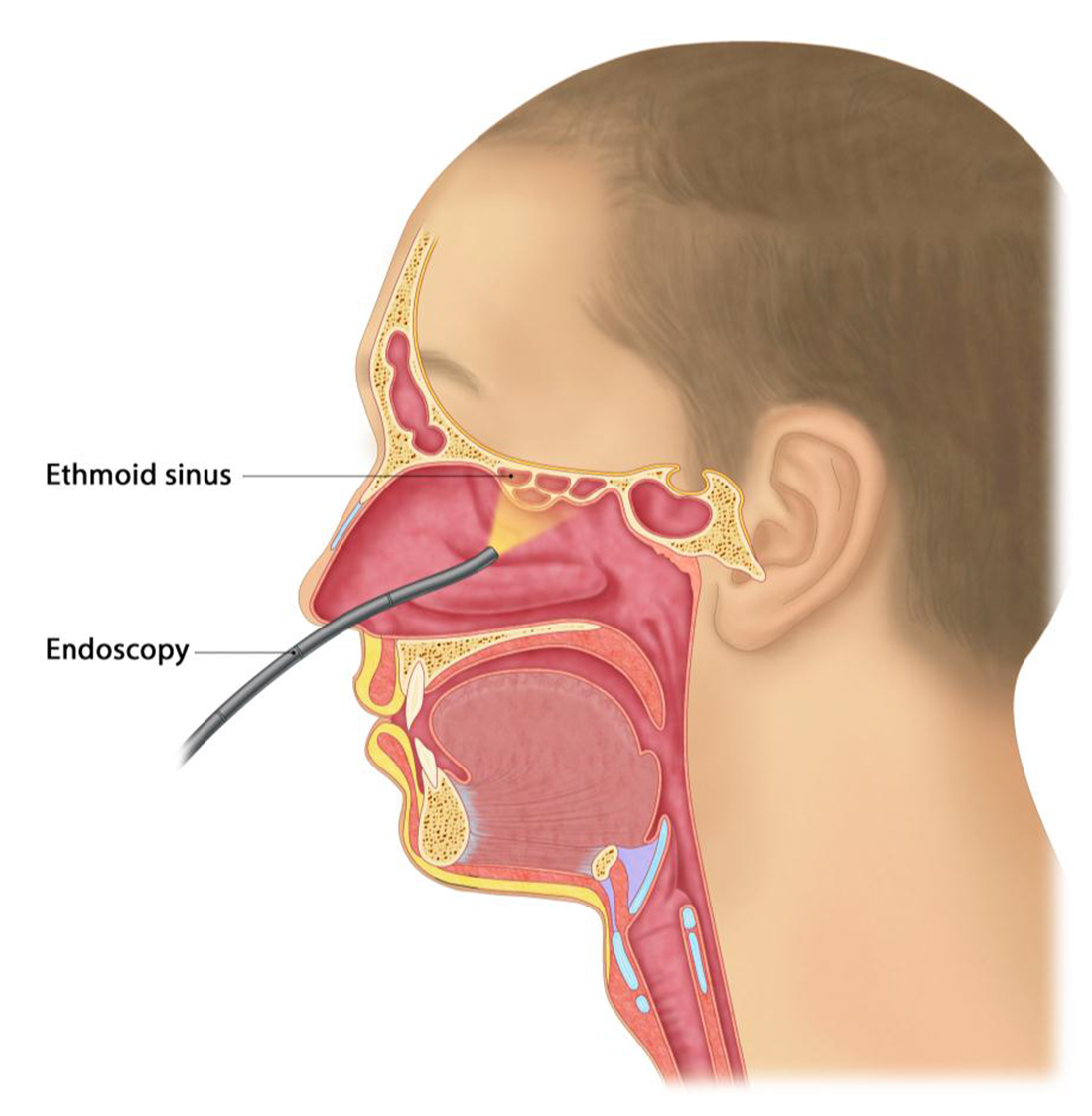
- or with a procedure called sinus endoscopy
- Sinus endoscopy is an office procedure in which a clinician uses a thin tube attached to a camera to see inside the sinuses (figure 4).
- Endoscopy also allows the clinician to take a sample of mucus from inside the sinuses to examine under the microscope, and identify bacteria, fungi, and other contributing factors.
- Samples of mucus from the front of the nasal cavity (which are easier to obtain) are not representative of what is found in the sinuses.
- Sinus Computed Tomography (CT) scan
Conditions Related to Chronic Rhino-Sinusitis:
- The linings of the nose and sinuses are similar to the linings of the lungs.
- Asthma:
- About one in five people with chronic rhinosinusitis also has asthma.
- The people most likely to have asthma are those who have chronic rhinosinusitis and nasal polyps.
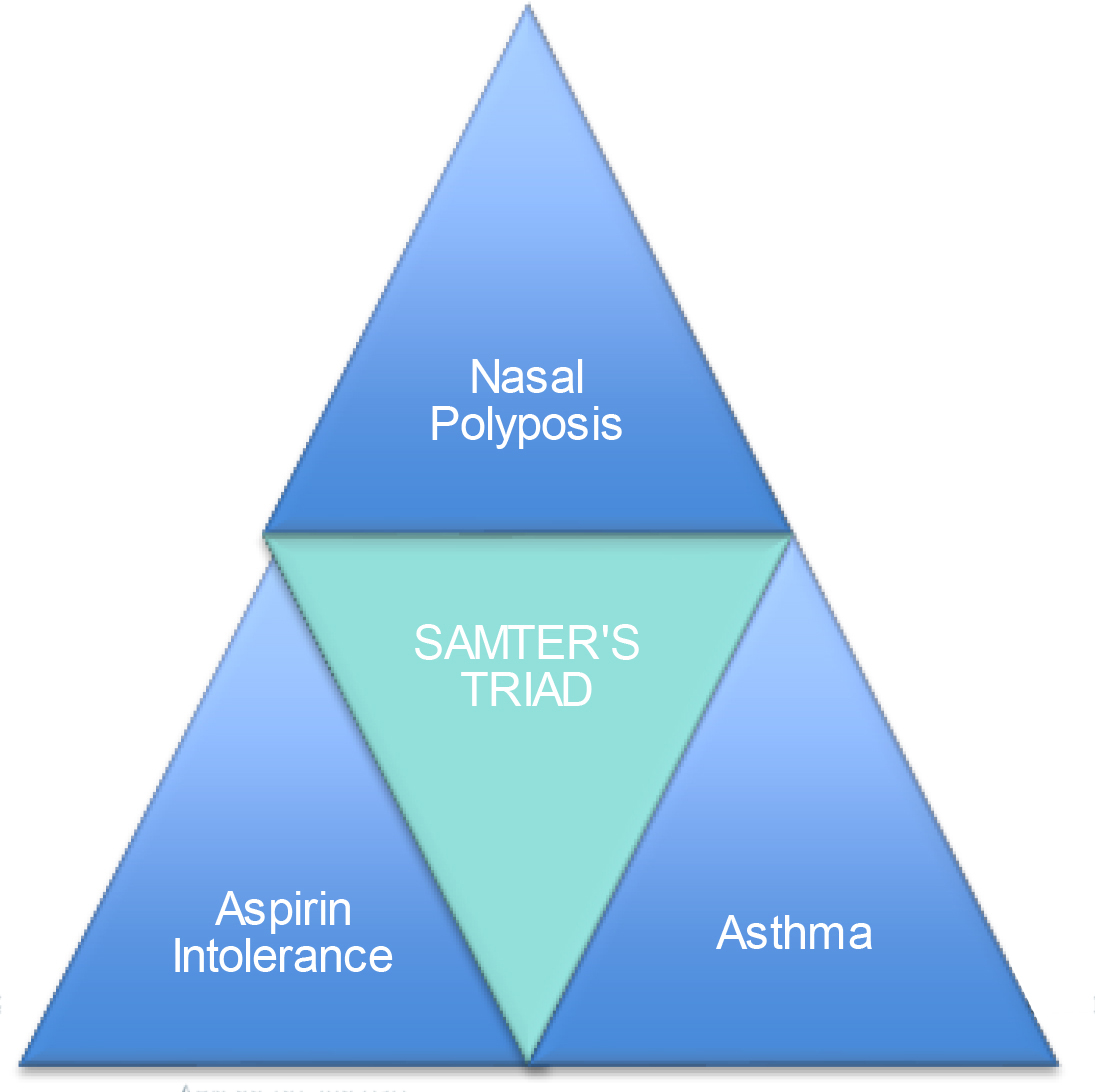
- Aspirin Exacerbated Respiratory Disease (AERD)
- Some patients with chronic rhinosinusitis, nasal polyps, and asthma also have a condition called aspirin intolerance, or Aspirin Exacerbated Respiratory Disease (AERD).
- Previously commonly referred to as Samter’s Triad (see below).
- The symptoms of aspirin intolerance consist of a noticeable worsening in nasal or chest symptoms in the first few hours after taking aspirin, ibuprofen, naproxen sodium, or other nonsteroidal anti-inflammatory drugs (NSAIDs).
- Worsening of symptoms may involve sudden nasal congestion, pain and pressure in the sinuses, wheezing, chest tightness, and cough.
- These reactions can be severe and even life threatening.
- In contrast, Paracetamol usually does not aggravate sinus and asthma symptoms.
- If you think you may have aspirin intolerance, you should avoid aspirin and other similar medications and talk to your MEG Surgeon, GP or Allergist.
- Some patients with chronic rhinosinusitis, nasal polyps, and asthma also have a condition called aspirin intolerance, or Aspirin Exacerbated Respiratory Disease (AERD).
Chronic Rhino-sinusitis Treatment
- Potential treatments for chronic rhinosinusitis include:
- Lifestyle modifications
- Smoking Cessation: People with chronic rhinosinusitis who smoke cigarettes should stop.
- Environmental Allergies: People who have environmental allergies as a contributing factor to their sinus problems may be able to change things in their home or work conditions to reduce exposure to the specific allergens that bother them. (See MEG Information pamphlet on Allergic Rhinitis and Specific Allergies)
- Daily nasal saline washing:
- Most people with chronic rhinosinusitis find that washing their nasal passages daily with saline (salt water) helps reduce symptoms.
- Washing the nose before applying medications also clears away mucus and reduces its interference with medications. (See MEG Information pamphlet on Saline Irrigation)
- Glucocorticoid nasal sprays, washes, and drops
-
- Because all forms of chronic rhinosinusitis involve some degree of inflammation i.e. irritation and swelling), most people with the condition need medications to reduce inflammation.
- Glucocorticoids (commonly called “steroids”) are very effective anti-inflammatory drugs.
- They also decrease mucus production and help shrink any polyps that may be present.
- Using glucocorticoids in form of nasal sprays or drops has the advantage of putting the medicine right where it is needed, and also of not treating the rest of the body, where the drug is not needed.
- Glucocorticoid Nasal Sprays: Your healthcare provider will probably ask you to try a glucocorticoid spray initially, as sprays are easy to use.
- Sprays however do not reach deep into the cavities of the sinuses, but they reduce swelling in the nasal passages and open up the areas through which the sinuses drain.
- Examples of steroid sprays include:
- triamcinolone acetonide (Nasacort®),
- budesonide (Rhinocort®),
- fluticasone (Flonase®),
- mometasone (Nasonex®)
- Glucocorticoid Nasal Washes or Drops: If the sprays do not seem to be working well enough, your provider may suggest switching to nasal drops, or adding a nasal glucocorticoid solution to the saline nasal wash.
- Nasal drops or washes help get the glucocorticoid solution higher up into the sinuses.
- If drops are prescribed, you must put them into the nose while lying in specific positions. This allows the liquid to move into the different sinuses (See MEG Information pamphlet on Nasal Sprays).
- In Australia, steroids do not come in nasal drops, but a medication called budesonide (Pulmicort® Respules) can be dissolved in saline and used as a nasal wash.
- Your MEG Health Professional will give you a prescription and specific instructions on how to use these medications.
- Glucocorticoid Tablets: In some cases, your MEG Healthcare Professional will recommend taking glucocorticoids (steroids) by mouth (orally). The most commonly used oral glucocorticoid is prednisone.
- Glucocorticoids taken orally get into the circulation and deliver higher doses of drug compared with nasal sprays, rinses, or drops.
- This can result in better treatment of the inflammation and more dramatic improvement in symptoms.
- However, glucocorticoids taken by mouth suppress normal immune responses throughout the body and can cause side effects, (See MEG Information pamphlet on Glucocorticoid use) so healthcare providers use them only when necessary.
- Your Meg Healthcare Professional will explain these possible risks and side effects when prescribing oral glucocorticoids. Also read information about Corticosteroids Side Effects
-
- Antibiotics:
- Although chronic rhinosinusitis is often caused by inflammation rather than infection, infection of the sinuses can develop and aggravate symptoms.
- As a result, some people need to take antibiotics.
- It is not unusual to need long courses of antibiotics, lasting several weeks, to fully treat a sinus infection in a person with chronic rhinosinusitis.
- Leukotriene modifiers:
- Healthcare providers occasionally prescribe a group of medications called leukotriene modifiers to people with chronic rhinosinusitis.
- These medications include:
- montelukast (Singulair®)
- These treatments work by reducing inflammation in a different way than glucocorticoids.
- These medications are not used for all types of chronic rhinosinusitis, and they appear to be most helpful for people with chronic rhinosinusitis with nasal polyposis who also have asthma +/- allergic rhinitis
- Biologics for Nasal Polyposis
- “Biologics” are synthetically prepared “monoclonal” antibodies designed to block a key element in the body’s immune system that contributes to inflammation.
- In Chronic Rhinosinusitis, these ‘blocking’ antibodies usually target a very focal part of the inflammatory pathway that is responsible for the changes in chronic rhinosinusitis and associated conditions such as asthma.
- The table below describes a few of the biologics currently approved in Australia and elsewhere for treatment of nasal polyps.
- These medications reduce the size of nasal polyps and improve the symptoms of chronic rhinosinusitis, when used in conjunction with a nasal steroid spray.
- The represent a significant advance in the treatment of nasal polyps, especially for patients who have had recurrence of nasal polyps despite sinus surgery.
- In Australia, most of these drugs currently require a co-diagnosis of significant asthma or eczema is required as a pre-requisite for patients to ‘qualify’ for the injection.
- There are numerous other biologics, currently in trial, that may become available in the years to come.
Generic Name Brand Name Mechanism of action Indication for Use Route of administration Frequency of Administrati on Possible side effects Mepolizumab Nucala® A Mono-clonal Antibody that selectively binds to and blocks human IL-5 CRS with Nasal Polyps which is: - Severe
- Eosino-philic
- recurrent post surgery
N.B. Only available in Australia through an ENT, Respiratory
Injection – into fat layer of skin (subcutaneous) Every 28 days, ongoing Injection site reactions
Headache
Back pain
Tiredness
Throat painDupilumab Dupixent® An Antibody that selectively binds to and blocks human Interleukin-4 and Interleukin-13 signalling, key drivers of allergic inflammation - Asthma
- Eczema
- Chronic Sinusitis with Nasal polyps
Injection – into fat layer of the skin (subcutaneous) on the top of the thigh, belly area, upper arm Every 2-4 weeks, ongoing Treatment effectiveness assessed 4 months after commencement
Injection site reactions Conjunctivitis
Omalizumab Xolair® An Antibody that selectively binds to and blocks human IgE (a natural antibody, that is a key driver of allergic inflammation) - Moderate – severe allergic asthma
N.B. Only available in Australia through a respiratory physician, immunologist, specialist pediatrician / physician
Injection – into fat layer of the skin (subcutaneous) on the top of the thigh, belly area, upper arm Every 2-4 weeks, ongoing Treatment effectiveness assessed 4 months after commencement
Injection site
reactions
Headache
Fatigue
Joint swelling
GI upset
HypotensionBenralizumab Fasenra® An Antibody that selectively binds to and blocks human IL-5ra, (a natural chemical and driver of allergic inflammation) - Eosinophilic asthma
N.B. Only available in Australia through a respiratory physician, immunologist, specialist paediatrician / physician
Injection – into fat layer of the skin (subcutaneous) on the top of the thigh, belly area, upper arm Every 4-8 weeks, ongoing Injection site reactions
Headache
Fatigue
Joint swelling
GI upset
Hypotension
Slight increased risk of parasitic infections
- Surgery:
- Although healthcare providers usually attempt to get the symptoms of chronic rhinosinusitis under control with medication first, some people need surgery to reopen the sinuses’ passages, and remove trapped mucus or polyps.
- Situations in which surgery is helpful include the following:
- When chronic rhinosinusitis symptoms do not improve enough with the medical treatments mentioned above, and there is evidence of persistent sinus disease on sinus computed tomography (CT) scan, such as complete blockage of one or more sinuses.
- When nasal polyps are present that do not sufficiently shrink with steroid treatment.
- When “allergic fungal rhinosinusitis” is suspected. Patients with allergic fungal rhinosinusitis usually have one or more sinuses that are completely blocked on the CT scan. Often these sinuses appear on the CT to be filled with thick, dense mucus that is difficult to remove in any other way except surgery. The surgery also allows for collection of samples of mucus, which are needed to confirm the diagnosis of allergic fungal rhinosinusitis.
- When there is severe deviation of the septum causing nasal blockage or other mechanical difficulty with sinus drainage.
- As discussed above, surgery can be very useful in the treatment of chronic rhinosinusitis, although by itself, it is rarely enough to control symptoms long term.
- The factors that caused the linings of the sinuses to become irritated and swollen and produce extra mucus in the first place must be addressed.
- In addition, because it is often impossible to eliminate these factors completely, most people require medications to control inflammation over time.
- Summary:
- Chronic rhinosinusitis cannot be cured in most cases, although treatment can significantly reduce symptoms and improve quality of life.
- The best approach to treatment involves identifying the factors that contribute to chronic rhinosinusitis in each specific person and correcting these factors to the degree possible.
- Most people are treated primarily with medications, although many also need surgery.
- Even after surgery, medications to control inflammation are usually needed indefinitely.
Concerns or questions?
You can contact your ENT Specialist at the Melbourne ENT Group (MEG):
- Phone: (03) 9994 1770
- Email: admin@melbentgroup.com.au
- Website: www.melbentgroup.com.au
Your GP is also the best contact for ongoing care and concerns.