Make an Appointment
Just fill out the form below to make an appointment to get help from our qualified staff of doctors. It’s easy and fast.
Who is this information for?
This information is for patients, families and carers following a diagnosis of Acute Otitis Media (AOM)
What is Acute Otitis Media (AOM)?
Middle-Ear infections, also called Otitis Media, are a common problem in children. About 50% of kids have ≥ 1 ear infection by their 1st Birthday.
Acute Otitis media is an infection of the middle section of the ear, (otitis = ear, media = middle). Most of the time it is caused by bacteria that nearly all children have in their nose and throat at one time or another.
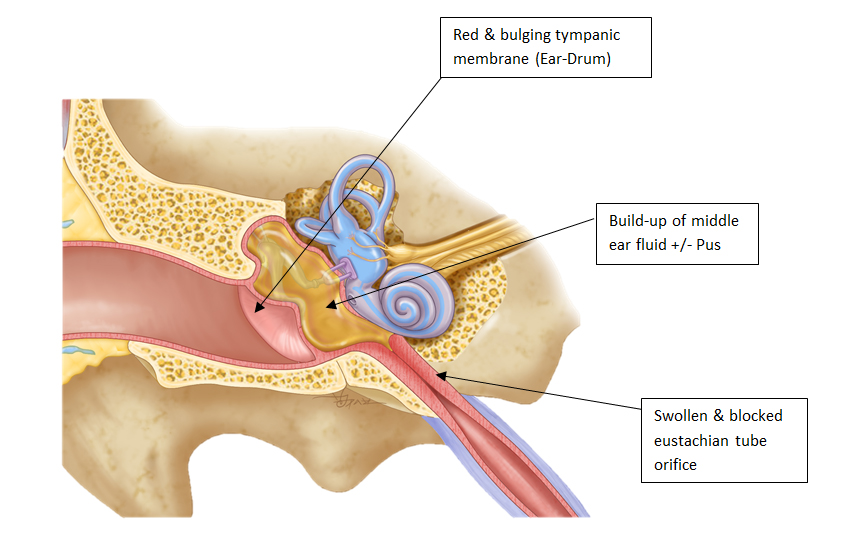
Ear infections most often develop after a viral upper respiratory tract infection (common old). These infections cause swelling of the lining of the nose and throat and also decrease normal defences against bacteria leading to an increased amount of bacteria in the nose. The nearby eustachian tube, which normally drains the middle ear into the back of the nose and maintains normal ear pressure, can also be impaired by viruses and bacteria
Fluid (called an effusion) may form in the middle ear and viruses and bacteria follow, resulting in inflammation in the middle ear.
Read more information about Middle Ear Aeration Techniques

What are the Symptoms of AOM?
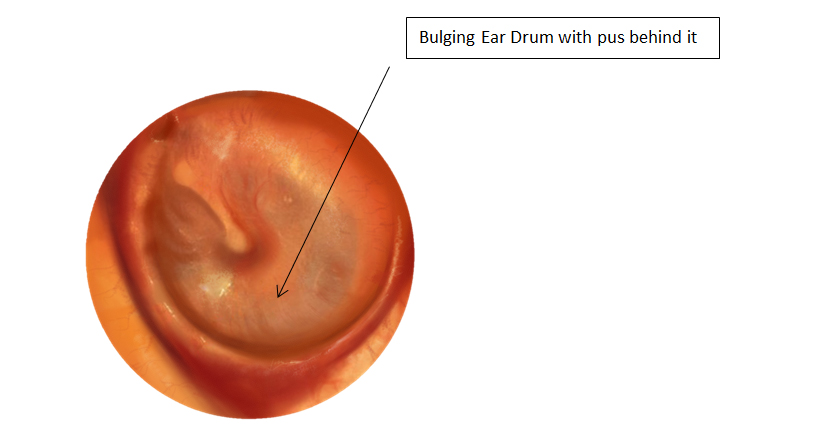
Most of the symptoms of AOM are due to the inflammation in the middle ear, and the resultant increased pressure and bulging of the ear drum.
In older children and adolescents symptoms may include an ear ache or pain, and temporary decreased hearing. These symptoms often come on fairly quickly.
In infants and young children, symptoms of an ear infection can include:
- Fever (temperature higher than 38°C)
- Pulling on the ear
- Irritability
- Less active, or flat
- Lack of appetite, difficulty eating
- Vomiting or diarrhoea
- Fluid draining from outer ear (clear, yellow, sometimes bloody)Patient Information for Otitis Externa and Discharging Ears
Acute otitis media can usually be diagnosed by your GP or ENT surgeon on the basis of the above symptoms and an examination of your child’s ear. Although the exam is not painful, most infants and children do not like having their ears examined. Your doctor will usually use an instrument (otoscope) or a light source and ear speculum (a small funnel used for looking into the ear) to examine the ear. Sometimes, wax and debris will need to be removed so that your doctor can get a good view of the ear drum.
Possible Complications of AOM:
- Ear drum (Tympanic Membrane) Rupture
One of the common complications of an ear infection is rupture (perforation) of the ear drum (tympanic membrane). This is due to the increased pressure of fluid build-up in the middle ear reducing blood flow to the ear drum and causing the tissue to weaken. It doesn’t hurt when the membrane ruptures, and many children actually feel better because pressure is released. Generally, a tympanic membrane rupture in this context heals very rapidly (within hours to days) once the infection has been treated, and generally without any long-term consequences. - Hearing Loss
The fluid that collects behind the eardrum (called an effusion – see above) can persists for weeks to months after the pain of an ear infection resolves. An effusion can cause trouble hearing, which is usually temporary. If the fluid persists, however, it may interference with speech and language development, and may require a hearing test and an ENT review to discuss further treatment options, such as Grommets. Read more information about Hearing Loss Strategies for Children.
Discharge Information: post Grommets Removal Surgery Recovery
- Recurrent AOM
Some children have numerous episodes of acute otitis media throughout the year, and this may have an impact on their school attendance, speech and learning progress, not to mention their well-being and quality of life. In such settings, it may be advisable to see an ENT to discuss possible preventative treatments, such as nasal sprays or Grommets.
What treatment is available?
Treatment of an ear infection may include any or a combination of: Observation & Supportive measures, Medications to treat pain and fever and/or Antibiotics, surgery
Prevention:
- Vaccines: Children should be vaccinated according to the national guidelines
- Pneumococcal Vaccine: In Australia, as in many countries, this includes the administration of the Pneumococcal Conjugate Vaccine. This vaccine targets one of the most common bacteria involved in ear, nose and throat infections in young children, Streptococcus Pneumoniae. Whilst the routine use of this vaccine provides only a modest protection against a child developing acute otitismedia (AOM), it does have a greater benefit in preventing the development of recurrent otitis media, and the need for Tympanostomy Tube (grommets) insertion.
- Influenza Vaccine: In Australia, Children aged 6 months are strongly recommended to receive the annual influenza vaccine, which protects against the seasonal ‘flu’ virus. Aside from children being at greater risk of significant illness and hospitalisation if they contract influenza, the vaccine can also provide a modest decrease in the chance of AOM during that year.
- Observation: In some cases, your child’s doctor or nurse will recommend that you watch your child at home before starting antibiotics. Observation can help to determine whether antibiotics are needed. Observation may be recommended in these situations:
- If your child is older than 24 months
- If ear pain and fever are not severe
- If your child is otherwise healthy
Supportive measures: Simple measures such as ensuring you child is well hydrated, and keeping your child cool if they are overheated, are key, as they are with any childhood illness.
Pain relief: The fever and pain of AOM can often be distressing for the child, and the rest of the family, so regular simple pain relief such as paracetamol and/or Ibuprofen is often advised. Always be sure to check the dosing requirements according to age and/or weight before administering these medications to infants.
Antibiotic Treatment: Many children get better without specific antibiotic treatment. However, antibiotics are routinely given to infants who have not responded to a period of observation (See above), or children who are less than 24 months old, have a high fever, infection in both ears, or have other medical problems.
Your doctor will usually prescribe an oral antibiotic which should be taken as directed. Antibiotics can have side effects such as diarrhoea or a rash. If you are concerned about side effects, you should contact your prescribing doctor. A course of 5-7 days is usually enough to resolve the infection, but sometimes longer courses or different antibiotics may be prescribed.
Uncommonly, if there is a hole in the ear drum and/or ear discharge, topical antibiotic drops may also be prescribed.
Surgical Treatment: Uncomplicated AOM does NOT need surgery. However, in rare cases, AOM may lead to local complications such as an abscess (collection of pus) behind the ear, or deeper inside. This may require surgical drainage.
See information about Glasgow Benefit Inventory
Also, some studies have demonstrated that the placement of middle ear ventilation tubes (Grommets) in patients who have had recurrent episodes of AOM, may decrease the chance of further episodes of AOM. For example, a child who has had ≥ 3 episodes of AOM in 6 months, or ≥ 4 episodes in 12 months, may be a candidate for grommets
This is also why follow-up with your doctor to ensure complete resolution of your child’s infection is also very important.
Complementary and Alternative Medical Treatments: There are a wide variety of complementary and alternative medical (CAM) treatments advertised to treat ear infections. These may include homeopathic, naturopathic, chiropractic and acupuncture treatments. There are few scientific studies or CAM treatments for ear infection, and even fewer studies that show CAM treatments to be effective. As a result, we don’t recommend these treatments for ear infections, especially in children.
Follow-up
Your child’s symptoms should improve within 24-48 hours whether or not antibiotics were prescribed. If your child does NOT improve after 48 hours, or gets worse, please call your doctor or return for advice.
Although fever and discomfort may continue even after the course of antibiotics has started, your child should improve every day.
Concerns or questions?
You can contact your ENT Specialist at the Melbourne ENT Group (MEG):
- Phone: 1300- 952-808
- Email: admin@melbentgroup.com.au
- Website: www.melbentgroup.com.au
Your GP is also the best contact for ongoing care and concerns.